If having fuller breasts would help you feel more feminine, beautiful, and confident, you’ve come to the right place! Breast augmentation is one of the most popular plastic surgery procedures that our experienced plastic surgeons perform here at Boston Plastic Surgery, and it’s also one of the most rewarding for our patients who choose to have the procedure.
We love to see our patients’ big smiles and happy faces after having breast augmentation. Our patients report benefits such as:
- Increased confidence about their body
- Positive impact on well-being
- Ability to fit better into clothes, bathing suits, etc.

As you do your research, you’ll find that there are quite a few decisions to make about your breast augmentation in Boston! The good news is that we’ll help you every step of the way, answering your questions and discussing your options in your consultation. We’ll help you make the choice that is best for you.
Your Breast Augmentation Consultation
Curious about what happens during a breast augmentation consultation at Boston Plastic Surgery? Join Dr. Phelan as she walks you through the entire process! In this video, she covers everything from discussing your aesthetic goals to reviewing your options for implants and placement.
Dr. Phelan is dedicated to ensuring you feel informed, comfortable, and confident in your choices. Whether you have questions about the procedure, recovery, or the results, she’s and the entire Boston Plastic Surgery team is here to guide you every step of the way.
Choosing Saline or Silicone Breast Implants
Is a desire for the most natural-feeling implant at the top of your list? Or do you want the smallest incisions possible? How much existing breast tissue do you have now? These are all questions that Dr. Samaha or Dr. Phelan will review during your consultation to help you choose what type of breast implants you would like to have: saline or silicone.
Silicone is a more popular choice due to its natural feel, but many patients decide that saline implants are better suited to their goals. What is most important is finding the right fit for your body.
Silicone Gel Breast Implants
Silicone breast implants are the most popular choice in the United States for breast augmentation. They quickly outpaced saline implants since their re-introduction in 2006, following a design improvement and FDA approval. Composed of a silicone shell filled with highly cohesive silicone gel, they closely mimic the characteristics of natural breast tissue. Some patients call them “gummy bear” implants.
Pros & Cons of Silicone Gel Implants:
- Silicone breast implants are generally smoother, softer, and lighter than saline implants.
- They have a softer, more natural feel and appearance.
- Silicone implants are less prone to rippling, and are well-suited to patients of all body types
- Since they come pre-filled from the manufacturer, silicone implants usually require a slightly larger incision. We still aim for the shortest incision possible, and this is facilitated by the use of devices like the “Keller Funnel”
- Routine monitoring is recommended to detect implant rupture. We offer Ultrasound imaging in our office, free of charge to our patients, according to the FDA-recommended schedule.
Saline Breast Implants
In the 1990s, the majority of breast augmentation surgeries used saline implants, as access to silicone implants was limited. The outer shell of a saline implant is made of a strong, flexible silicone shell and the inside is filled with saline, a sterile saltwater solution.
Since the re-introduction and FDA approval of silicone implants, fewer women choose saline implants these days, as they have significant limitations. Dr. Samaha or Dr. Phelan will help you decide at your personal consultation.
Pros & Cons of Saline Implants
- They are slightly heavier and firmer, and feel less natural than silicone gel breast implants.
- Saline implants can be more prone to visible wrinkling, particularly in thinner patients with little natural breast tissue to cover the implant.
- Because they are filled during surgery, saline implants can provide some adjustability in implant volume.
- Should the contents of the implant enter the body for any reason, the body can safely absorb the saline.
- If the saline implant ruptures, it is noticeable right away as that breast will deflate. No additional ultrasound or MRI imaging is required to monitor breast implants beyond routine mammograms.
New! Motiva silicone breast implants
We are thrilled to be one of the first plastic surgery practices in Boston to offer Motiva® breast implants – the latest FDA-approved silicone implant option for breast augmentation and breast implant exchange.
If you are considering breast augmentation or breast implant replacement, Motiva’s innovative design, natural feel, and advanced safety features may be the ideal choice to achieve your aesthetic goals.
How we ensure your safety at Boston Plastic Surgery
Are silicone breast implants safe?
Even now, after FDA approval, misinformation still prevails about silicone implants. The truth is, silicone breast implants were used widely from 1963 to 1992, in literally millions of patients. During this time, they had some design flaws which caused some local problems. However, media reports that tried to correlate connective tissue diseases with the use of silicone breast implants were not backed by scientific evidence.
In 2006, the restrictions were lifted based on new, re-designed “cohesive gel” implants, and surgeons once again are able to utilize silicone implants. With the improvements in silicone implant technology, several excellent options are now on the market.
Keller Funnel Certified

An advancement in silicone breast augmentation delivery, the Keller Funnel™ is a soft, sterile device that many plastic surgeons use throughout the United States. Because the Keller Funnel reduces necessary incision size, it allows for more precise implant placement and reduces the risk of implant damage. Learn more »
Breast Implant Sizing: Getting to the right size takes a personalized approach
This is what many patients consider to be the fun part of their breast augmentation process: choosing what size they want to be.
With all of the advancements in implant technology, we now have an unprecedented array of choices. Silicone gel and saline implants come in a variety of shapes and sizes. Dr. Samaha and Dr. Phelan begin the implant sizing process by first concentrating on what you would like the end result to look like. If you have goal photos to share with us at your consultation that helps us to understand your vision and design a surgical plan tailored to you.
We will help you narrow down your choices based on three major factors:
- Your desired breast size after surgery
- Your individual anatomy: height, weight, chest width, and other important measurements
- Your current breast size, shape, and degree of symmetry
Choosing Breast Implant Size
During the consultation, we will first make sure to understand the size and shape that you would like to achieve. We then take measurements, which are used to guide the choice of implant type, shape, and size. We make every effort to help our patients get a realistic idea of what they will look like after surgery. We incorporate personalized breast implant sizing to help our patients choose the ideal implant size.
Choosing Implant Profile
Implants come in a variety of “profiles,” ranging from wide low-projecting implants to “High Profile” implants with a relatively narrower diameter. The choice is made based on your desired outcome, tissue characteristics, and natural breast dimensions. A mastopexy or breast lift performed at the time of augmentation is another factor influencing profile choice.
When do we prefer round implants and when does we prefer shaped?
With all the new shaped implant options available, you may wonder which implant makes the most sense for you. Dr. Samaha and Dr. Phelan will recommend smooth round implants or teardrop-shaped implants depending on your goals and your anatomy.
Incision options for safety and scar-minimizing techniques
There are several techniques that Dr. Samaha or Dr. Phelan can utilize for the placement of implants. No matter which incision option is chosen, rest assured your scars will be:
- Difficult to detect by anyone except you and perhaps a close partner
- Easily hidden beneath clothing, even a bikini
- Made as small as possible
With proper care, your scars should also fade significantly over the first year following surgery. Our staff will provide you with all the information you need regarding breast augmentation recovery and aftercare, including scar care.
Breast Implant Placement: Over or under the muscle?
During breast augmentation surgery, breast implants are placed under the breast tissue or beneath the chest wall muscle. With either location, the implants will be properly centered under the nipple. The two placement options are defined as the following:
- Subfascial placement: under the breast tissue and under the lining of the pectoralis muscle, but over the muscle itself.
- Submuscular placement: below breast tissue and partially beneath the pectoralis muscle. This is commonly known as a “dual-plane” technique, as the muscle would cover the upper portion of the implant.
The placement option chosen will be largely determined by the patient’s body type, tissue thickness, and lifestyle requirements. There are benefits and disadvantages associated with each location, but they differ in each case, so your plastic surgeon will discuss your options thoroughly in your consultation.

Dual Plane Breast Augmentation (Under the Muscle): Pros & Cons
For this placement option, the lower part of the pectoralis major muscle is released from the chest, and this muscle covers the top portion of the breast implant. This option:
- Provides better coverage for the upper portion of the implant, which is helpful in patients with thinner tissues.
- Reduces the chance of visible rippling and implant palpability (ability to feel the implant edges) in some aspects of the breast, but not so much in the lower and outer aspects, where there would be no muscle coverage.
- May help to visualize the breast tissue during a mammogram
This technique requires patience during the recovery period while the implants “settle” into their final position, which can take a few months. Additionally, you may notice some movement of the implant when you flex your chest muscles.
Subfascial Augmentation (Over the Muscle): Pros & Cons
Subfascial implant placement has regained favor among surgeons and patients. There is a growing consensus that its safety profile is similar to dual-plane augmentation. For many patients, this technique offers an easier recovery and less risk of the breast twitching or moving with activity or exercise, which is known as an animation deformity. In subfascial placement, the pectoralis major muscle is left intact, and just the thin lining over the muscle (fascia) is elevated to cover the implant. Not every patient is a candidate for this technique, particularly if your tissues are very thin.
Breast Surgery Recovery: We want you to enjoy your new look as soon as possible!
At Boston Plastic Surgery, we use techniques that can greatly reduce the postoperative discomfort of this surgery. Many of our patients need to use very little (if any) narcotic pain medication, thus avoiding potential side effects and experiencing an easier recovery.
What to Expect During Recovery
After breast augmentation, it is normal to feel tired and sore. During your recovery, you will wear a soft, supportive surgical bra. You are able to shower after 48 hours. Most patients experience minor soreness and are able to go about their normal activities–except for lifting– shortly after surgery. Swelling, bruising, and changes in skin sensation are also normal and should subside in the weeks that follow.
Returning to Normal After Breast Augmentation
Every patient heals at a slightly different rate, but in general, you can expect to return to your usual activities after your surgery along the following timeline:
- Rest at home the first 1 to 2 days after surgery.
- Shower 2 days after surgery; follow your post-op instructions!
- Depending on the activity level required for your job, returning to work may be possible within a few days.
- Wear a soft, supportive bra (sports bra) for the first several weeks
- Gradually return to exercise after 3 to 4 weeks
Your breasts may be sensitive to direct stimulation for about three weeks, so avoiding physical contact is recommended. Ask your plastic surgeon when you should resume any exercise and normal physical activity.
Scars from breast augmentation will be firm and pink for six weeks or longer. They will gradually flatten out and fade over time, becoming less and less noticeable. Breast augmentation scars are well-concealed in the natural contours of your breast and/or easily hidden by clothing. Scar management techniques are available to speed the scar healing process and minimize the appearance of scars. Scar management is customized based on your skin type and your history of scar healing.
Long Term Considerations
Routine mammograms should be continued after breast augmentation for women who are in the appropriate age group. The mammography technician will use a special technique to ensure that you get a reliable reading. Most imaging centers are well-equipped and experienced in performing mammograms on women with breast implants, but be sure to tell the physician ordering your mammogram and your mammography technician that you have had breast augmentation.
For silicone breast augmentation, it is recommended to obtain a breast ultrasound or MRI first 5-6 years after surgery and then every 2-3 years thereafter to detect implant rupture. Many women have no symptoms if there is an implant rupture, so this monitoring is important. We perform complimentary in-office breast ultrasounds for our breast augmentation patients, making your post-augmentation monitoring as simple and easy as possible.
If you need more details about recovery from breast augmentation, contact Boston Plastic Surgery to schedule a consultation with Dr. Samaha or Dr. Phelan.
We hope you find this information helpful! Feel free to contact us or call our office at 617.786.7600 if you have any questions.
FAQs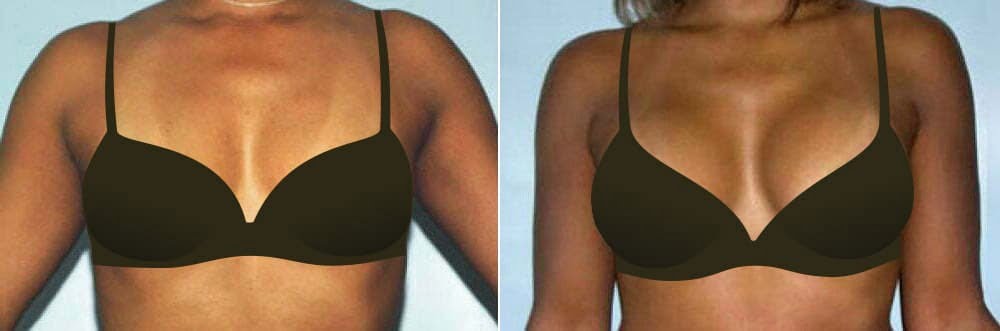
More Breast Augmentation Techniques
Fat transfer to the breast
Fat transfer breast augmentation (also known as “Butterfly” breast augmentation) is an excellent choice for women who are interested in improving their breast shape and adding a small amount of volume, but prefer to avoid a breast implant.
Fat is harvested from the abdomen or thighs, processed, and grafted to the breasts in layers to improve shape and cleavage. Approximately 60% of the fat grafted takes, and the percentage of fat that takes stays permanently.
After 1-2 months, initial swelling and minor bruising resolve, and final results are visible. Fat grafting can also be performed more than once to add additional volume if desired.
Breast asymmetry correction
If you have breast asymmetry, breast asymmetry correction may be customized to your anatomy and goals and included in your procedure plan:
- For many patients, this may mean a breast lift/breast reduction on one or both sides, removing different amounts of tissue from each side to adjust volume differences.
- For patients who want to add volume, this may mean differential breast implant sizing. Fat grafting can also be used to treat breast asymmetry, and may require more than one session to achieve the desired result.
It is important to understand that it is never possible to achieve perfect symmetry. Breasts are always asymmetric to some degree both before and after surgery, but correction can offer improvement.
Tuberous breast correction
Tuberous breast is a congenital difference that features a high breast fold (below the breast); a narrow, constricted breast shape; small breast size; and areolar herniation (puffiness of the nipple). Women may have some or all of these features, and the condition frequently presents with significant asymmetry, as well.
This is most commonly treated with a combination breast implant and a breast lift through a periareolar incision approach. This condition may require more than one stage for surgery, depending on your anatomy.
- Key Benefits
- Glossary
- Enhanced breast size and shape
- Improved body proportions
- Correction of asymmetrical breasts
- Restored breast volume post-pregnancy
- Enhanced cleavage and fullness
- Augmentation Mammaplasty/Augmentation Mammoplasty: Medical terms for breast implant surgery, a procedure to enhance the size and shape of a woman’s breasts.
- Micromastia: A condition where an individual has underdeveloped breast tissue, often leading to small breasts.
- Underdeveloped Breast Tissue: Breast tissue that has not fully developed, often resulting in a smaller breast size.
- Small Breasts: Breasts that are smaller in size, which some individuals may seek to enhance through breast augmentation.
- Asymmetrical Breasts: A condition where one breast is a different size or shape than the other, often corrected through breast augmentation surgery.
- Boob Job: A colloquial term for breast augmentation surgery, aimed at increasing breast size or improving breast shape.
- Breast Enhancement/Breast Enlargement: Procedures aimed at increasing the size and improving the shape of the breasts, typically involving breast implants.
- Flat Chest: A term used to describe very small breasts or a chest with little to no breast tissue.
- Breast Implant Illness (BII): A term used to describe a range of symptoms that some women believe are related to their breast implants, including fatigue, pain, and cognitive issues.
- Breast Cancer: A disease in which malignant cells form in the tissues of the breast, sometimes leading to the need for breast reconstruction surgery.
- Autologous: Referring to the use of the patient’s own tissue in reconstructive surgery, such as using fat grafts for breast augmentation.
- Anaplastic Large Cell Lymphoma (ALCL): A rare type of cancer that can develop around textured-surface breast implants (these implants are rarely used today).
- Breast Augmentations/Breast Augmentation Surgery: Procedures to enhance the size and shape of the breasts using implants or fat grafts.
- Breast Implant Prosthesis: An artificial device implanted into the breast to increase size or improve shape.
- Breast-Implants: Medical devices placed inside the breast to increase its size or alter its shape.
- Breast Milk: Milk produced by the mammary glands of a woman, production of which can be affected by certain types of breast surgery. Talk with your surgeon before breast augmentation about the ideal surgical plan to support breastfeeding if you plan to breastfeed after surgery.
- Breast Reconstruction: Surgery to rebuild the shape and look of a breast, often after mastectomy due to breast cancer.
- Breast Size/Breast Volume: The overall dimensions or fullness of the breast, often enhanced through augmentation.
- Breast Tissue: The tissue that makes up the breast, including glandular and fatty components.
- Capsular Contracture: A potential complication of breast augmentation where scar tissue forms around the implant, causing it to harden.
- Chest Muscles: Muscles located in the chest area, which can affect breast implant placement and support.
- Cosmetic Surgeon/Cosmetic Surgery: A medical professional and practice focused on enhancing a person’s appearance through surgical procedures, including breast augmentation.
- DIEP Flap/TRAM Flap: Types of breast reconstruction techniques using tissue from the lower abdomen.
- Fat Grafts/Fat Tissue: The transfer of fat from one part of the body to the breasts to enhance size and shape.
- General Anesthesia: A medically induced state of unconsciousness used during breast augmentation surgery.
- Grafts: Tissues transplanted from one part of the body to another, used in some breast augmentation and reconstruction procedures.
- Healthcare Provider: The professionals involved in providing medical care, including those performing breast surgeries.
- Hospital: A medical facility where surgical procedures, including some breast augmentations, are performed.
- Implant Procedure: The surgical insertion of breast implants to enhance breast size and shape.
- Mammogram/Mammographic: Imaging tests used to screen for breast cancer, which can be tailored to you if you have breast implants.
- Medical Complications: Potential adverse effects or issues arising from breast augmentation surgery.
- Pectoralis Muscle: The muscles of the chest that can be involved in the placement of breast implants.
- Pocket: The surgically created space in the breast where an implant is placed.
- Prosthetic Breast: An artificial breast form used in reconstruction after women undergo mastectomy.
- Recipient Site: The area of the body where tissue or implants are placed during surgery.
- Reconstruction: The process of rebuilding the breast’s shape and size, often after cancer surgery.
- Shape/Size: The form and dimensions of the breast, which are key considerations in breast augmentation.
- Silicone Breast Implants/Silicone Implants: Implants filled with silicone gel used to enhance breast size and shape.
- Subglandular Placement: Positioning of a breast implant above the chest muscle and below the breast tissue.
- Surgical Procedure/Surgical Training: The operations performed to enhance breast size and the specialized education required to perform these surgeries.
- Tissue/Tissue Expander: The cells and materials making up the breast, and a device used to stretch the skin and tissue before placing a permanent implant.
- Transverse Rectus Abdominis Myocutaneous (TRAM) Flap: A type of breast reconstruction using tissue from the lower abdomen.
- Volume: The amount of space the breast occupies, often increased through augmentation.
References »
Coroneos CJ, Selber JC, Offodile AC 2nd, Butler CE, Clemens MW. US FDA Breast Implant Postapproval Studies: Long-term Outcomes in 99,993 Patients. Annals of Surgery. 2019 Jan;269(1):30-36. doi: 10.1097/SLA.0000000000002990.
Swezey E, Shikhman R, Moufarrege R. Breast Implant Rupture. 2023 Jan 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–.
Eisenberg T. The Underappreciated Saline Breast Implant. Aesthetic Plastic Surgery. 2023 Apr;47(2):897-900. doi: 10.1007/s00266-022-03106-z.
Adams WP Jr, Mckee D. Matching the Implant to the Breast: A Systematic Review of Implant Size Selection Systems for Breast Augmentation. Plast Reconstr Surg. 2016 Nov;138(5):987-994. doi: 10.1097/PRS.0000000000002623.
Christopher R. Costa, Kevin H. Small, William P. Adams, Bra Sizing and the Plastic Surgery Herd Effect: Are Breast Augmentation Patients Getting Accurate Information?, Aesthetic Surgery Journal, Volume 37, Issue 4, 1 April 2017, Pages 421–427, https://doi.org/10.1093/asj/sjw221
Hadad E, Sualhi I, Legarda C, Seligman Y, Sorkin A, Dor O, Menashe S, Heller L, Wiser I. Silicone breast implant rupture is more prevalent in the dominant limb side: A retrospective cohort study. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2023 May;80:126-132. doi: 10.1016/j.bjps.2023.02.016.
Guimier E, Carson L, David B, Lambert JM, Heery E, Malcolm RK. Pharmacological Approaches for the Prevention of Breast Implant Capsular Contracture. Journal of Surgical Research. 2022 Dec;280:129-150. doi: 10.1016/j.jss.2022.06.073.
Quinlan CS, Lynham R, Kelly JL. Risk Factor Analysis for Capsular Contracture, Malposition, and Late Seroma in Subjects Receiving Natrelle 410 Form-Stable Silicone Breast Implants. Plast Reconstr Surg. 2017 Sep;140(3):499e. doi: 10.1097/PRS.0000000000003613.
Newman AN, Davison SP. Effect of Keller Funnel on the Rate of Capsular Contracture in Periareolar Breast Augmentation. Plast Reconstr Surg Glob Open. 2018 Jun 18;6(6):e1834. doi: 10.1097/GOX.0000000000001834.
Headon H, Kasem A, Mokbel K. Capsular Contracture after Breast Augmentation: An Update for Clinical Practice. Arch Plast Surg. 2015 Sep;42(5):532-43. doi: 10.5999/aps.2015.42.5.532.
Risks and Complications of Breast Implants. U.S. Food & Drug Administration.
FDA Strengthens Safety Requirements and Updates Study Results for Breast Implants. U.S. Food & Drug Administration.
Ri C, Yu J, Mao J, Zhao M. Trends in Breast Augmentation Research: A Bibliometric Analysis. Aesthetic Plast Surg. 2022 Dec;46(6):2691-2711. doi: 10.1007/s00266-022-02904-9.
Coroneos CJ, Selber JC, Offodile AC 2nd, Butler CE, Clemens MW. US FDA Breast Implant Postapproval Studies: Long-term Outcomes in 99,993 Patients. Ann Surg. 2019 Jan;269(1):30-36. doi: 10.1097/SLA.0000000000002990.
Cohen BE, Biggs TM, Cronin ED, Collins DR Jr. Assessment and longevity of the silicone gel breast implant. Plast Reconstr Surg. 1997 May;99(6):1597-601.
Shen Z, Chen X, Sun J, Chiu C, Yu Y, Lin X, Zhang Z, Xu J. A comparative assessment of three planes of implant placement in breast augmentation: A Bayesian analysis. J Plast Reconstr Aesthet Surg. 2019 Dec;72(12):1986-1995. doi: 10.1016/j.bjps.2019.09.010.
Brown MH, Shenker R, Silver SA. Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery. Plast Reconstr Surg. 2005 Sep;116(3):768-79; discussion 780-1. doi: 10.1097/01.prs.0000176259.66948.e7.
To learn about your breast augmentation options, schedule a consultation with one of our skilled plastic surgeons, Dr. Samaha or Dr. Phelan, by calling 617-786-7600.